
WARNING: Some images might prove upsetting to viewers.
Pressure ulcers, aka pressure sores or bed sores, normally develop of the bony areas of the body like the heels, hips or cheek bone, ankles, ears, elbows, etc.. These sores are caused by lying down or sitting in the same position for a long time. If there is pressure on your skin for too long, it can cut off the blood supply to the area. The skin gets weak and can die without enough blood. Pressure ulcers are a serious problem. Bedridden people or those confined for very long periods of time in stationary chairs or in wheel chairs are in danger of developing these sores.
Pressure ulcers can occur even in under the best care conditions and are not necessarily an indication of neglect. Total prevention of these wounds from occurring has not been proven to be possible. Nevertheless, because these ‘injuries’ can lead to disfigurement and /or infection, their development on the skin must always be looked for and their presence addressed immediately.

Pressure wound prevention is a top concern of knowledgeable and loving caregivers and professional care staff. These skin care concerns have been a source of major concern and dread as they can lead to survey citations and even litigation. It is true that pressure sores are sometimes associated with factors such as neglect, inadequate staffing or poor nutritional care.
Certified Nursing Assistants (CNAs) and Certified Personal Care Aides (PCAs) are critical in skin care and wound detection. It is important they they have current clinical knowledge, tools, support and ongoing education about this subject. As Senior Care Auditors are increasingly used by families as independent care quality assessors to check up on care attendants, attention to the care and management of the skin of those who choose to age at home can be better monitored and more quickly reported, in cases of neglect.

Senior Care Auditing is one of the few 21st century fast growing career paths. Find out more about Senior Care Auditing and the Senior Care Auditor career at CertifiedCare.org.
CHANGES IN TERMINOLOGY AND THE LAW
In recent years there have been some innovations in wound care prevention and management, but communication and team cooperation (if there is a team) are ideal paths to successful treatment. NPUAP, the National Pressure Ulcer Advisory Panel, serves as the authoritative voice for improved patient outcomes in pressure injury prevention and treatment through public policy, education and research. Recently this organization replaced the term “pressure ulcer” with “pressure injury”. This change is creating quite a stir It is contended by the group that the change in terminology more accurately describes pressure injuries to both intact and ulcerated skin.
Many practitioners are concerned about the new nomenclature because of issues with lawsuits related to the language. It is feared that Attorneys might wrongly suggest or conclude that injury implies fault.
New Definitions
What is a pressure injury?

A pressure injury is localized damage to the skin and/or underlying soft tissue usually over a bony prominence or related to a medical or other device. The injury can present as intact skin or an open ulcer and might be painful. The injury occurs as a result of intense and / or prolonged pressure or pressure in combination with shear. the tolerance of soft tissue for pressure and shear may also be affected by micro-climate, nutrition, perfusion, comorbidities, and condition of the soft tissue.
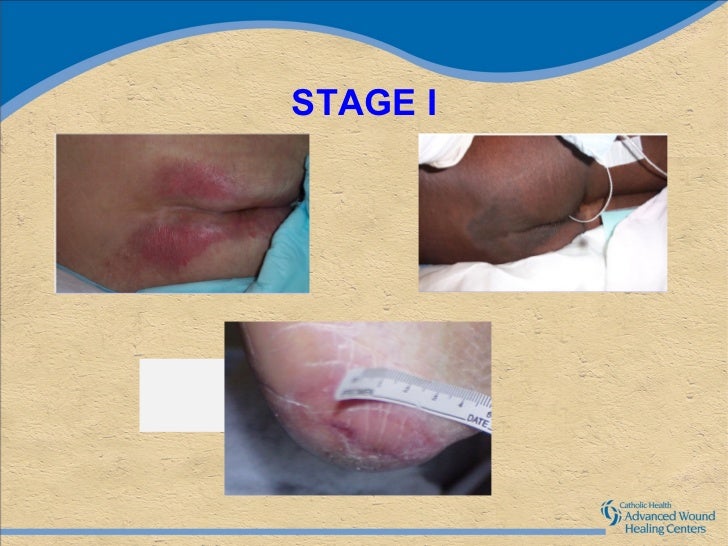
STAGE 1 PRESSURE INJURY This is defined as a non-blanchable erythema of intact skin. Intact skin with a localized area of non-blanchable erythema, which might appear differently in darkly pigmented skin. Presence of blanchable erythema or changes in sensation, temperature, or firmness might precede visual changes. Color changes do not include purple or maroon discoloration; these might indicate deep tissue pressure injury.
Get certified now as a Senior Care Auditor and earn 5 certifications for 1 all inclusive low price only at CertifiedCare.org.
STAGE 2 PRESSURE INJURY Presents as partial-thickness skin loss with exposed dermis. The wound bed is viable, pink or red, moist, and might also present as an intact or ruptures serum-filled blister. Adipose (fat) is not visible, and deeper tissues are not visible. Granulation tissue, slough, and eschar are not present.
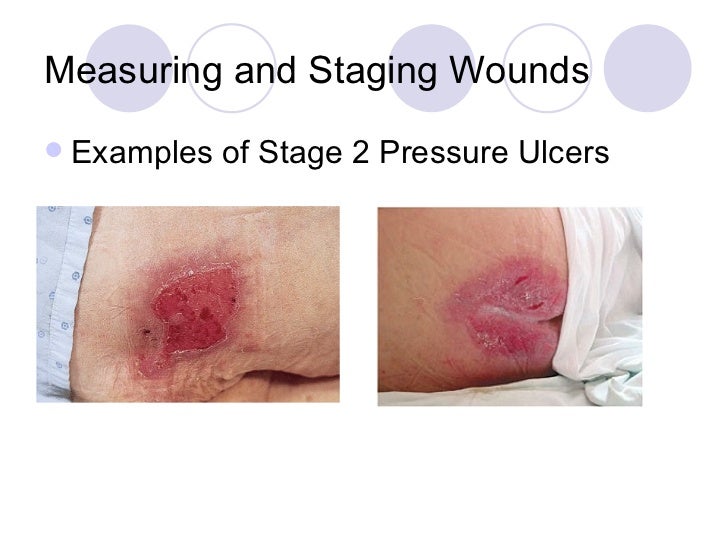 These injuries commonly result from adverse micro-climate and shear in the skin over the pelvis and shear in the heel. This stage should not be used to describe moisture-associated skin damage, including incontinence-associated dermatitis, intertriginous dermatitis, medical adhesive-related skin injury, or traumatic wounds (skin tears, burns, abrasions).
These injuries commonly result from adverse micro-climate and shear in the skin over the pelvis and shear in the heel. This stage should not be used to describe moisture-associated skin damage, including incontinence-associated dermatitis, intertriginous dermatitis, medical adhesive-related skin injury, or traumatic wounds (skin tears, burns, abrasions).
STAGE 3 PRESSURE INJURY Presents as full thickness skin loss, in which adipose (fat) is visible in the ulcer and granulation tissue and epibole (rolled wound edges) are often present. Slough and / or eschar might be visible.
 The depth of tissue damage varies by anatomical location; areas of significant adiposity can develop deep wounds. Undermining and tunneling might occur. Fascia, muscle, tendon, ligament, cartilage, and/or bone are not exposed. If slough or eschar obscures the extent of tissue loss, this is an Unstageable Pressure Injury.
The depth of tissue damage varies by anatomical location; areas of significant adiposity can develop deep wounds. Undermining and tunneling might occur. Fascia, muscle, tendon, ligament, cartilage, and/or bone are not exposed. If slough or eschar obscures the extent of tissue loss, this is an Unstageable Pressure Injury.
STAGE 4 PRESSURE INJURY Full-thickness skin and tissue loss with exposed or directly palpable fascia, muscle, tendon, ligament, cartilage, or bone in the ulcer. Slough and /or eschar might be visible. Epibole (rolled edges) , undermining, and /or tunneling often occur. Depth varies by anatomical location. If slough or eschar obscures the extent of tissue loss, this is an Unstageabe Pressure Injury.

Families and friends use Certified and registered Senior Care Auditors to make sure your loved one is getting the skin care attention they deserve. Become a certified senior care auditor today!
UNSTAGEABLE PRESSURE INJURY obscured and full thickness skin loss in which the extent of tissue damage within the ulcer cannot be confirmed because it is obscured by slough or eschar.
DEEP TISSUE PRESSURE INJURY (DTPI) Intact or non-intact skin with localized area of persistent non-blanchable deep red, maroon, purple discoloration or epidermal separation revealing a dark wound bed or blood-filled blister. Pain and temperature change often precede skin color changes. Discoloration may appear differently in deeply pigmented skin. This injury results from intense and /or prolonged pressure and shear forces at the bone-muscle interface. The wound may evolve rapidly to reveal the actual extent of tissue injury, or might resolve without tissue loss. If necrotic tissue, subcutaneous tissue, granulation tissue, fascia, muscle, or other underlying structures are visible, this indicates a full-thickness pressure injury (Unstageable, Stage 3 or Stage 4). Do not use DTPI to describe vascular, traumatic, neurpathic, or dematologic conditions.
RELATED PRESSURE INJURY DEFINITIONS
MEDICAL DEVICE RELATED PRESSURE INJURY Medical device related pressure injuries result from the use of devices designed and applied for diagnostic or therapeutic purposes. The resultant pressure injury generally conforms to the pattern or shape of the device. The injury should be staged using the staging system.
MUCOSAL MEMBRANE PRESSURE INJURY This type of injury is found on mucous membranes with a history of medical device in use at the location of the injury. Due to the anatomy of the tissue, the injuries cannot be staged.
Senior Care Auditing is one of the few 21st century fast growing career paths. Find out more about Senior Care Auditing and the Senior Care Auditor career at CertifiedCare.org.
Source: www.npuap.org/national-pressure-ulcer-advisory-panel
